Over the past few years, there has been a push to stop hemorrhages in the civilian trauma world. The Stop the Bleeding course (www.stopthebleed.org) has been made readily available through the internet and is an excellent place to start. Beyond that, other Traumatic injuries often don’t get publicity. During the war, recognizing and managing these wounds are critical to ensure casualties can survive. This article will explain some of the wounds of war and things to consider in management and triage.

Whether it's from a bullet, or shrapnel from an explosion, treating a traumatic limb injury is one of the easier wounds to address.
Traumatic Injury: Limbs
There are essentially three types of reasons for a traumatic limb on the battlefield as it relates to projectiles. The first is from a bullet, whether it be a handgun or a rifle round. Unless it hits a major artery or organ, the damage is usually something that can be triaged. The second is from a larger projectile like shrapnel. The problem with these is that multiple fragments are involved in the blast. This makes the repair of the wound more challenging. The last type is like that from an improvised explosive device (IED). These have enough energy to amputate the limb involved. These pressure-detonated blasts often contain dirt and debris, making them more challenging to clean and treat.
Medical classes have recently become more available to the civilian population to help with such treatment scenarios (www.7ccrt.org). Tactical Combat Casualty Care classes are a great place to start your training. It isn’t always about putting on a tourniquet and “calling it good.” We need to know when to put it on, and more recently, data suggesting when to convert the tourniquet to a lower-level dressing. The logistics of war may not mean you get to triage right away and will need to care for the casualty for a prolonged period of time. We are starting to see Prolonged Field Care classes that are also incredibly insightful (see RECOIL OFFGRID Issue 53).

Treating chest wounds can be tricky, especially when it’s impossible to use a tourniquet to control bleeding.
Traumatic Injury: Chest Wounds
Several types of chest wounds can occur in trauma; however, it will be delineated here as penetrating chest trauma versus blunt-force trauma. As for penetrating chest trauma, like from a bullet or a knife, we are taught to “seal the box.” Place a chest seal, preferably a vented chest seal, over the wound and watch for good or bad changes in the patient's condition. The two types of injury patterns seen with penetrating trauma are pneumothorax and tension pneumothorax.
This hole in the chest wall and/or lung can disrupt the physiologic mechanisms that allow us to breathe effectively. A tension pneumothorax is life-threatening and should be recognized and treated immediately. The importance of the vented chest seal, or burping the non-vented seal, cannot be overstated. There are classes readily available to help distinguish these two types of penetrating injuries and how to treat them.
In blunt-force chest trauma, the mechanism of injury becomes important to understand. A motor vehicle accident may cause blunt-force trauma from the seatbelt alone. Other times, the vehicle impacting the body can cause trauma. Fractured ribs could potentially cause a pneumothorax; it’s important to remember this upon your evaluation.
Higher levels of blunt-force trauma, like from blast injuries, can have a delayed onset of symptoms. The patient may have shortness of breath, cough, coughing up blood, and chest pain. In this case, the lungs will fill up with blood and fluids, exacerbating the shortness of breath. The other thing with blast injuries to the lung is that there are often blast injuries to different body parts (e.g., brain, ears, eyes, abdomen), which should also be evaluated.
There are four patterns of blast injuries to consider. The primary blast injury is from the over-pressurization of the blast itself. Secondary blast injury is from fragments of debris and projectile that enter the wound. Tertiary blast injuries occur from being thrown from the explosion. This is where head trauma can be seen apart from the initial percussion blast. Quaternary blast injuries are from the burns, smoke, chemicals, and toxins in the reaction to the blast aftermath. These injuries will need immediate treatment followed by triage to higher levels of care.

head injury is obvious, but there doesn’t need to be a visible sign for damage to the brain to occur.
Traumatic Injury: Brain
We use terms like “shellshock,” concussion, closed head injury, and traumatic brain injury to describe any situation where the brain is shaken, not stirred. This can be from a projectile or a blast injury. Fortunately, the government is taking more credence into our military member's complaints of headaches, confusion, change in consciousness, and subsequent psychological issues.
It was estimated that during the Iraqi wars, 25 percent of soldiers suffered some form of mild traumatic brain injury due to exposure to repeated blast injuries, perhaps by sending rounds downrange. For some soldiers, the blast would occur from an IED or incoming round and cause the casualty to leave their feet. This would invariably cause the soldier to strike their head as a tertiary impact from the blast and lead to traumatic brain injury.
With further research, there’s now some evidence that traumatic brain injury has both neurological and psychological lasting effects.
The latter part has developed into what we are now calling post-traumatic stress disorder (see RECOIL OFFGRID Issue 43). While the effects of PTSD can vary widely, there are many therapies that can at least be offered to provide some relief. Unfortunately, cognitive therapies and standard medications (like sertraline and paroxetine) have only been about 50-percent effective in reducing symptoms. Off-label use of prazosin has varied potential for benefit, especially with respect to night terrors.
One medication that is being considered due to its significant effect on hard-to-treat depression is ketamine. This is a drug that would typically be used to put someone to sleep with anesthesia before surgery. There have been anecdotal reports that it’s helpful in people with traumatic brain injury as well as PTSD. Reviews of the literature also say it’s relatively safe to administer in these patients.
Traumatic Injury: Inhalation
The vivid pictures of the World Trade Center coming down with billowing smoke and debris littering the area serve as a poignant example of a quaternary blast injury pattern. This occurs when debris, heat, chemicals, and toxins infiltrate the lungs and cause respiratory distress. Since 9/11, there have been more deaths associated with the victims and first responders than the original bloodbath itself. These fatalities have been linked to various cancers, mental health, and breathing issues.
Perhaps the most common inhalation injury is that of smoke inhalation and the toxic chemicals from the burning matter. Nearly one-third of those exposed to fire will suffer from inhalation injury. The injury pattern is usually more in the upper airway, where swelling, fluids, and tissue damage occur.
This prevents adequate air movement to the lower levels of the lungs, where we can exchange oxygen for carbon dioxide. The more chemicals that are spread by the fire, the deeper they can penetrate the lungs and cause damage at the alveolar level. Chemicals such as ammonia and sulfur dioxide can cause further tissue damage and impede gas exchange, which is essential for normal respiration.
In milder cases, they may heal within a few days. Most of the moderate-to-severe patients will need airway support via intubation or tracheotomy and, once intubated, higher levels of care. These people will often die from respiratory failure or pneumonia.
This color-coded diagram from Dark Angel Medical makes remembering which treatment goes where much easier.
Traumatic Injury: Burns
Fire has been weaponized throughout the millennia. From shrapnel wounds causing minor burns to penetrating projectiles trapping service men and women in personnel carriers and causing extensive burns, burn management has been at the forefront of the war. As the burn progresses from a superficial first-degree burn (like a sunburn) to a third-degree deep burn, management becomes more complex. The third-degree burn has denuded all the skin, which acts as a protective barrier from infection and debris.
The skin also serves as a barrier to prevent fluid loss, and without the protection, the fluid loss from oozing and evaporation can be extensive, depending on the size of the burn.
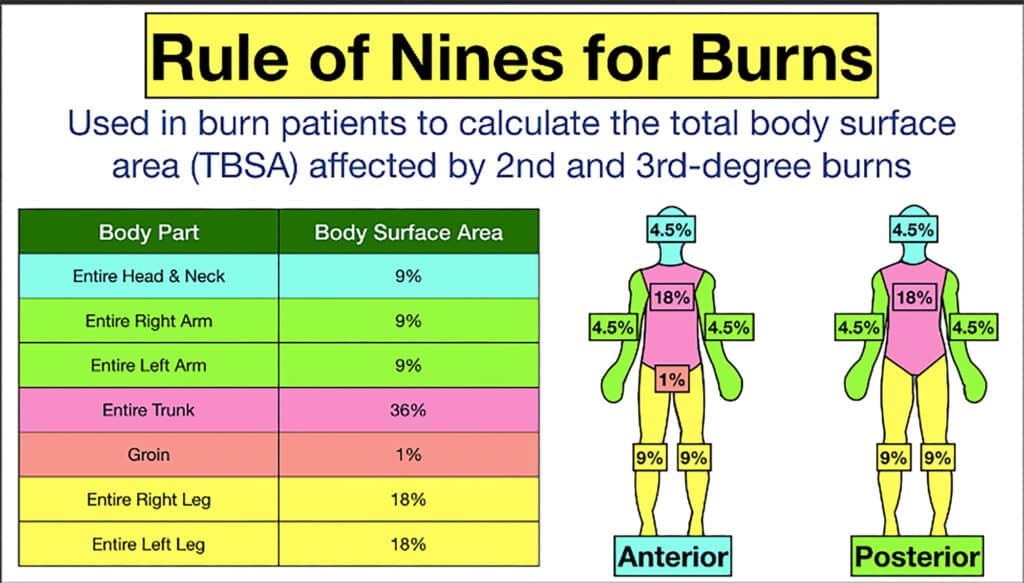
One way we determine the extent of a burn is to determine its total body surface area. We use a Rule of Nines to assess second- and third-degree burns. The head and each arm are considered 9-percent involved. The legs are considered 18-percent each (9-percent anteriorly and 9-percent posteriorly). The thorax is considered 36 percent and can be broken down into anterior and posterior (18 percent) and further by chest and abdomen (9-percent each). Fluid resuscitation should be 2-4mL per kilogram of ideal body weight per total body surface area of burn involved over the first 24 hours.
Burn dressings will help keep moisture from evaporating as quickly as possible. Water-Jel makes a great product and is available to cover the areas exposed by the Rule of Nines. Silvadene cream is an antibiotic-impregnated cream that provides a barrier over the burn and helps control infection. If the casualty has a delay in transport to higher levels of care, this would be a good option. And don’t forget about pain control.
In Conclusion
The examples above should encourage more understanding of injury patterns in war. It’s not meant to be a comprehensive review but to bolster your underlying fund of knowledge. With an internet search, you should be able to find classes to help increase your repertoire should the need arise. Once you find a training cadre you like, stick with them.
Information changes and evolves in the medical world; keeping up with those changes is essential. Some great things are being done on the management side, which is making a difference in saving civilians, first responders, and our servicemen and women.
About the Author
David L. Miller, DO FACOI, is an internist in private practice for 20 years. His experiences away from the office have included time as a fight doctor in regional MMA events and as a team physician for 10 years at a mid-major university in the Midwest. Currently, he serves as the lead medical instructor for the Civilian Crisis Response team based out of Indianapolis.
Sources
Read More
Don’t miss essential survival insights—sign up for Recoil Offgrid's free newsletter today!
Check out our other publications on the web: Recoil | Gun Digest | Blade | RecoilTV | RECOILtv (YouTube)
Editor's Note: This article has been modified from its original version for the web.
The post Traumatic Injury: Wounds of War appeared first on RECOIL OFFGRID.
By: Nick Italiano
Title: Traumatic Injury: Wounds of War
Sourced From: www.offgridweb.com/preparation/traumatic-injury-wounds-of-war/
Published Date: Thu, 28 Nov 2024 12:00:39 +0000
------------------------
Did you miss our previous article...
https://bushcrafttips.com/bushcraft-news/bug-out-when-to-beat-feet
 What is BushcraftSurvival SkillsToolsVideosBushcraft CampsBushcraft KitsBushcraft ProjectsPrivacy PolicyTerms And Conditions
What is BushcraftSurvival SkillsToolsVideosBushcraft CampsBushcraft KitsBushcraft ProjectsPrivacy PolicyTerms And Conditions
